When we think about healthy aging, we often focus on mobility, strength, and independence, but brain health plays an equally critical role. One emerging area of research gaining attention is the glymphatic system, the brain’s natural cleaning and detox network that works primarily during sleep.
Understanding the glymphatic system in seniors can shed light on the hidden links between sleep quality, dementia risk, nighttime confusion, and even fall safety. This guide breaks down the science in simple terms and explains why it matters not just for cognitive health, but for everyday safety and peace of mind.
What Is the Glymphatic System?
The glymphatic system is essentially the brain’s built-in waste removal system. Throughout the day, normal brain activity generates toxins and metabolic byproducts, including proteins associated with neurodegenerative diseases.
If these substances aren’t cleared efficiently, they can accumulate over time and potentially affect cognitive health. A helpful way to picture it is as the brain’s overnight cleaning crew.
Just as the body relies on the lymphatic system to remove waste from tissues, the brain relies on the glymphatic system to flush out debris using cerebrospinal fluid that circulates between brain cells.
This nightly “rinse cycle” is one reason restorative sleep is so important. Interestingly, scientists only identified and described this system in 2012, which explains why many people—even those focused on healthy aging—are still unfamiliar with it.
Yet as research grows, the glymphatic system is becoming a key piece of the puzzle in understanding sleep, brain health, and aging.
How the Glymphatic System Works During Sleep
The glymphatic system is most active during deep sleep, especially slow-wave sleep. During this phase:
- Brain cells shrink slightly
- Fluid flow between cells increases
- Waste clearance becomes more efficient
This process is often described as the brain’s “detox cycle” during sleep. One of the primary substances cleared is beta-amyloid, a protein strongly associated with Alzheimer’s disease.
When sleep is fragmented or insufficient, this cleansing process is disrupted, leaving the brain with less time to remove accumulated waste. That’s why the glymphatic system and sleep are so closely intertwined; quality sleep directly supports the brain’s long-term cognitive health.
Why It Slows Down With Age
As we age, both sleep patterns and brain physiology begin to change, and these shifts can quietly affect how the glymphatic system works. The system depends heavily on deep, restorative sleep, which naturally declines over time.
Several age-related changes can slow glymphatic efficiency, including:
- Reduced time spent in deep (slow-wave) sleep
- Changes in blood vessel elasticity that affect fluid movement
- Slower circulation of cerebrospinal fluid
- Higher rates of insomnia and other sleep disorders
According to the National Institute on Aging, older adults tend to experience lighter, more fragmented sleep, which may limit the brain’s ability to complete its nightly repair and cleanup processes.
Over time, this helps explain why aging and brain health are so closely linked to sleep quality and why protecting sleep becomes increasingly important in later years.
The Link Between Poor Sleep and Dementia Risk
A growing body of research is revealing a strong connection between chronic sleep disruption and long-term cognitive decline. Scientists are increasingly looking at sleep not just as rest, but as a protective factor for brain health.
Studies suggest that:
- Reduced slow-wave (deep) sleep may accelerate cognitive decline
- Poor sleep may contribute to increased amyloid buildup in the brain
- Chronic insomnia is associated with a higher risk of Alzheimer’s
The Alzheimer’s Association identifies sleep as a modifiable risk factor, meaning it’s one area where lifestyle changes may help support long-term brain health. While poor sleep alone does not cause dementia, persistent disruption can create conditions that make the brain more vulnerable over time.
For families and caregivers, this makes the relationship between sleep and dementia risk especially important. That’s why improving sleep may not only support cognition but also reduce safety risks that often emerge alongside nighttime cognitive changes.
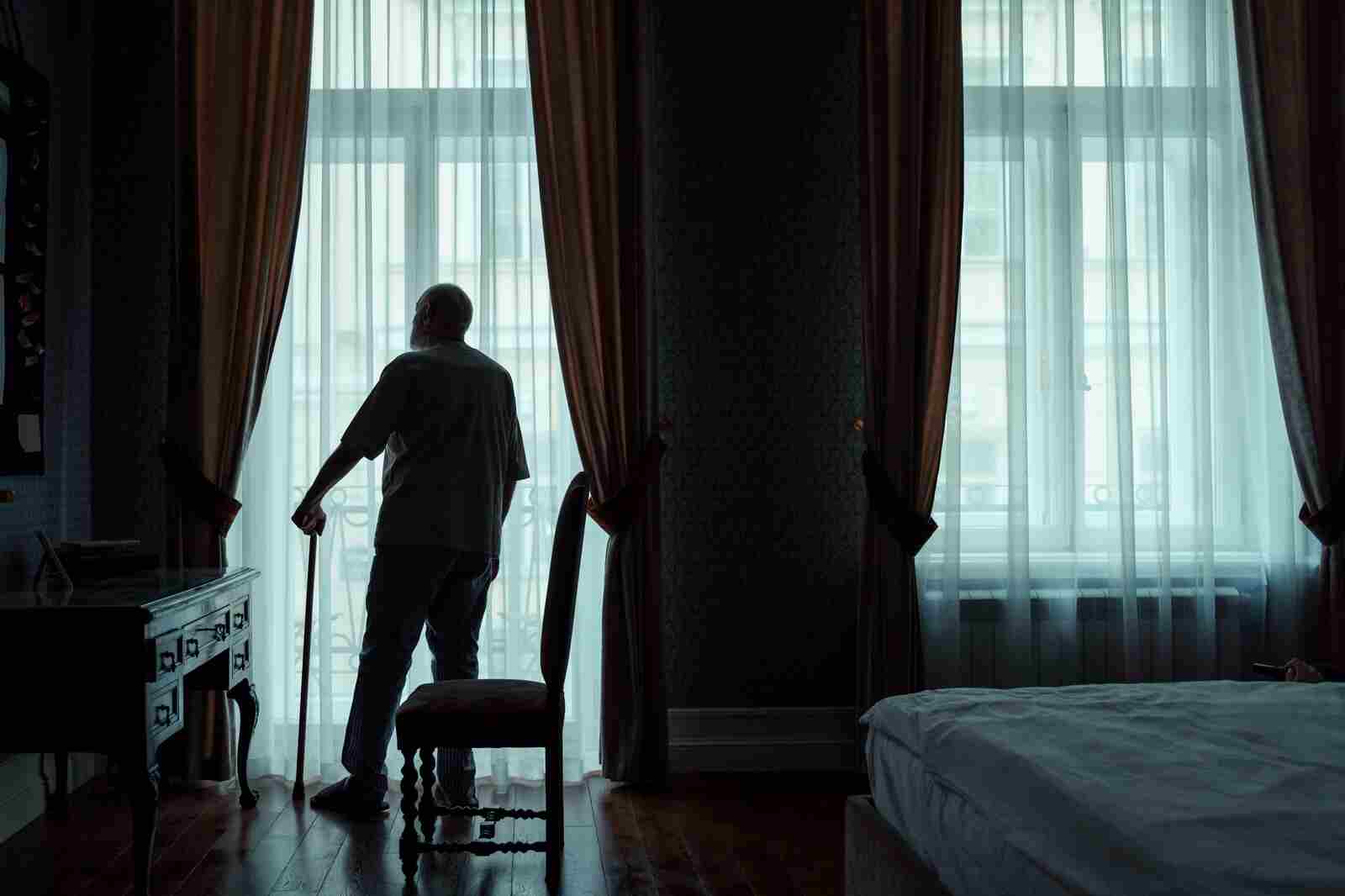
Nighttime Confusion, Wandering & Fall Risk in Seniors
Sleep disruption in older adults is not just a cognitive concern; it’s also a safety issue.
Poor glymphatic function often correlates with:
- Nighttime confusion (sundowning)
- Disorientation after waking
- Wandering behavior
- Poor balance at night
These factors significantly increase senior fall risk at night, especially in low-light environments. Bathroom trips, dehydration, or sleep inertia can compound risk. Nighttime falls are particularly dangerous because they often involve:
- Delayed discovery
- Hard flooring surfaces
- Limited supervision
Understanding this connection reframes sleep issues as both a neurological and a safety concern.
How Families Can Reduce Nighttime Emergency Risks
While families cannot directly control the glymphatic system, they can meaningfully reduce the risks that often accompany poor sleep and nighttime confusion. Small, practical adjustments can improve both sleep quality and overnight safety.
Improve sleep quality
Healthy sleep habits support brain recovery and may help stabilize nighttime cognition.
- Maintain a consistent sleep and wake schedule
- Limit evening screen exposure and bright lights
- Create a calm, comfortable sleep environment (cool, dark, quiet)
Enhance nighttime safety
The physical environment matters since many falls occur when seniors wake disoriented.
- Install motion-activated lighting in bedrooms, hallways, and bathrooms
- Keep walking paths clear of clutter or loose rugs
- Use non-slip flooring or traction mats in high-risk areas
Monitor behavioral changes
Subtle shifts in nighttime behavior can signal rising cognitive or safety risks.
- Increased confusion or agitation after dark
- Wandering or nighttime restlessness
- New or worsening sleep disturbances
These adjustments reduce both cognitive strain and injury risk by addressing the most common triggers of nighttime incidents. For additional protection, many families adopt a layered safety strategy that includes 24/7 medical alert monitoring, especially when seniors live alone, experience nighttime disorientation, or are at higher risk of falls.
This ensures that if something does happen overnight, help is immediately accessible.
When Poor Sleep Becomes a Safety Concern
Occasional sleep disruptions are normal. But certain patterns signal elevated risk:
- Frequent nighttime wandering
- Repeated falls or near-falls
- Sudden confusion after waking
- Increased nighttime bathroom accidents
- Unexplained bruises or injuries
At this stage, sleep is no longer just a comfort issue; it becomes an emergency preparedness concern. If your loved one experiences confusion at night, having instant access to help can make all the difference.
Solutions that provide emergency response support at home, such as wearable alert systems, ensure assistance is available even when a phone isn’t. These tools don’t replace medical care, but they shorten response time, which is one of the strongest predictors of recovery after nighttime falls.
Why This Matters for Families
The glymphatic system highlights an important truth: sleep is not passive. It is an active, essential maintenance process for brain health.
When sleep declines with age, the effects can ripple outward:
- Cognitive vulnerability
- Nighttime confusion
- Increased fall risk
- Greater caregiver stress
Recognizing these connections allows families to shift from reactive care to proactive safety planning, especially during nighttime hours when risks are highest.
FAQs
Does the glymphatic system decline with age?
Yes. Research suggests glymphatic efficiency decreases with age due to lighter sleep, vascular changes, and reduced slow-wave sleep. This decline may contribute to toxin buildup and increased cognitive vulnerability over time.
How does sleep affect dementia risk?
Sleep plays a key role in clearing brain waste, including proteins linked to Alzheimer’s disease. Chronic sleep disruption has been associated with higher dementia risk, although it is one of many contributing factors.
Understanding the glymphatic system in seniors provides a powerful lens for viewing brain health, sleep quality, and nighttime safety as deeply interconnected. While improving sleep supports cognitive health, preparing for nighttime risks ensures seniors stay safe, giving families greater peace of mind.